
Daniel Mordes, MD, PhD
Our lab aims to elucidate the mechanisms of neurodegeneration in ALS and related diseases and to establish better models of neurodegenerative diseases with the goal of creating paths forward for the development of targeted therapies. We are based in new research facilities at the Weill Institute for Neurosciences.
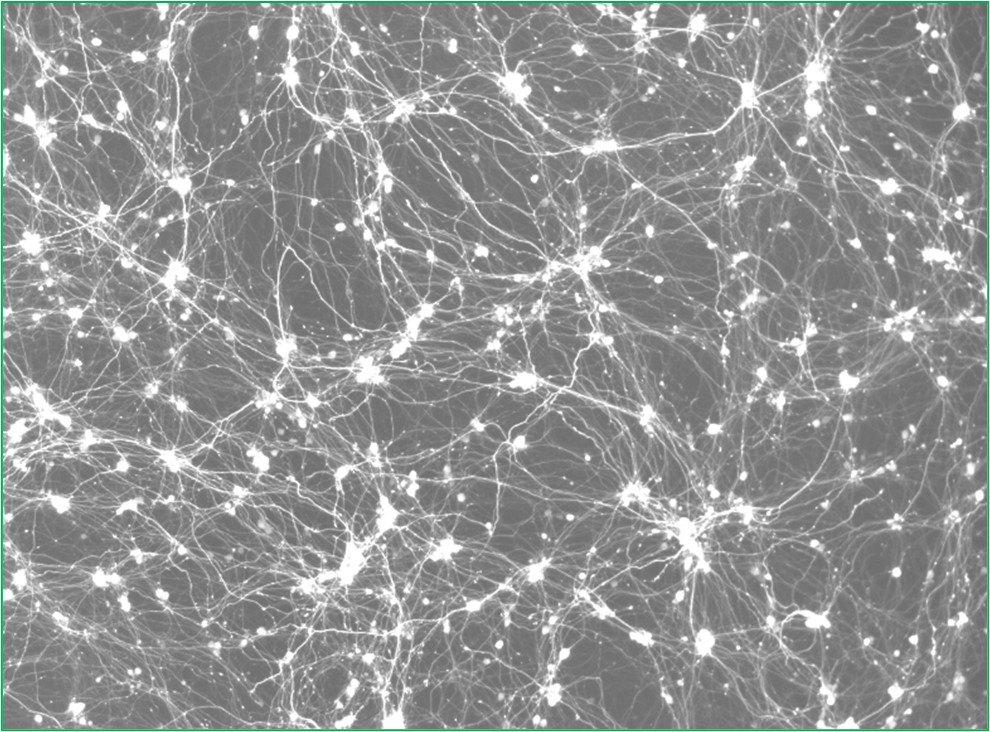
The most common cause of ALS, which affects motor neurons, and frontotemporal dementia (FTD) is a hexanucleotide (GGGGCC) repeat expansion within an intron of C9ORF72, which encodes a protein that likely functions in endo-lysosomal pathways. This repeat expansion is transcribed into repetitive RNAs that sequester RNA binding-proteins and undergoes non-canonical translation into dipeptide repeat proteins in the absence of an ATG start codon. We are working to determine how these dipeptide proteins cause cellular toxicity and contribute to disease pathogenesis using stem cells to generate the neuronal populations that are affected in disease. This research integrates a combination of transcriptomic and proteomic approaches as well as single-cell technologies to examine patient brain samples.
Additionally, we seek to delineate how protein homeostasis pathways function in human neurons as loss-of-function variants in genes encoding protein chaperones and autophagy proteins are associated with ALS and related neurological diseases. The Mordes lab has also studied movement disorders characterized by the accumulation of alpha-synuclein in collaboration with members of the Prusiner lab. We are interested in defining the transcriptional changes in alpha-synuclein-associated neurodegeneration as a guide to studying disease mechanisms in neuronal and glial cells.
Dr. Mordes is a neuropathologist and primary investigator in the Institute for Neurodegenerative Diseases at the University of California, San Francisco. He completed clinical training in neuropathology at Massachusetts General Hospital and then performed post-doctoral studies with Kevin Eggan at Harvard University and the Broad Institute. In the Eggan lab, he studied how both loss-of-function and gain-of-function mechanisms associated with a hexanucleotide repeat expansion in C9ORF72 contribute to ALS in mouse and human stem cell-derived models as well as patient nervous system tissue samples. Prior to being recruited to UCSF, he was on the faculty of Harvard Medical School. He has served as a clinical neuropathology fellow for the Massachusetts Alzheimer’s Disease Research Center and as a neuropathologist for the Harvard Brain Tissue Resource Center.
